As part of the adjudication process, claims are either approved, denied, or require more information. This results in a range of manual tasks which must occur to manage appeals from patients or providers, investigations, and administration of denials — creating a cost center within the revenue management cycle.
Instabase for Appeals and Denials
Instabase automates document understanding for all documents included in the appeals and denials process, regardless of document type or format, to streamline an end-to-end workflow.

Processing Appeals and Denials
Why Instabase?
The Instabase Platform helps health insurance payors during the adjudication process by leveraging deep learning for document understanding, increasing accuracy and reducing processing time.
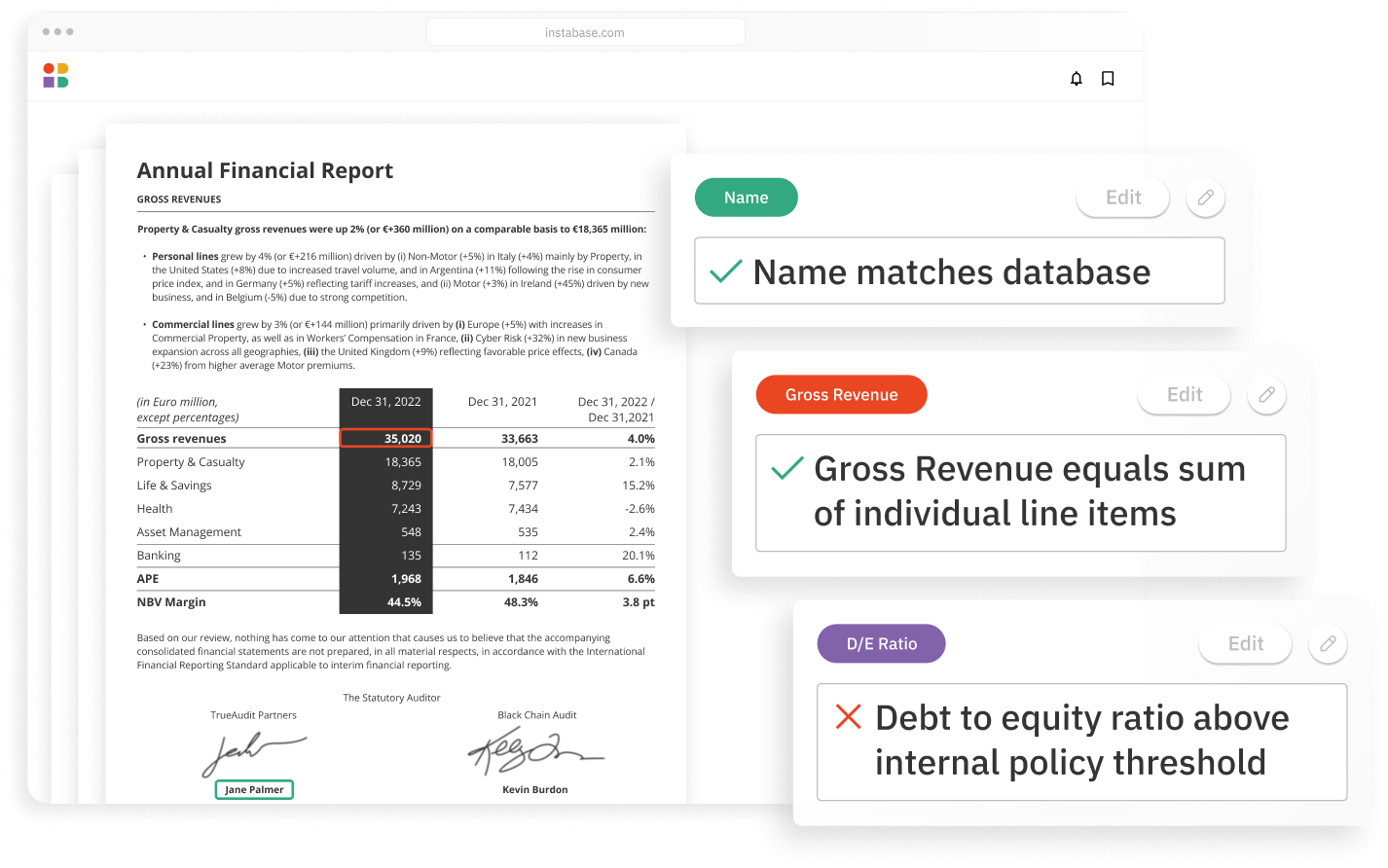
Accurately automate any document type
- Highly accurate extraction
- Any structure, any language
- Handwriting & printed
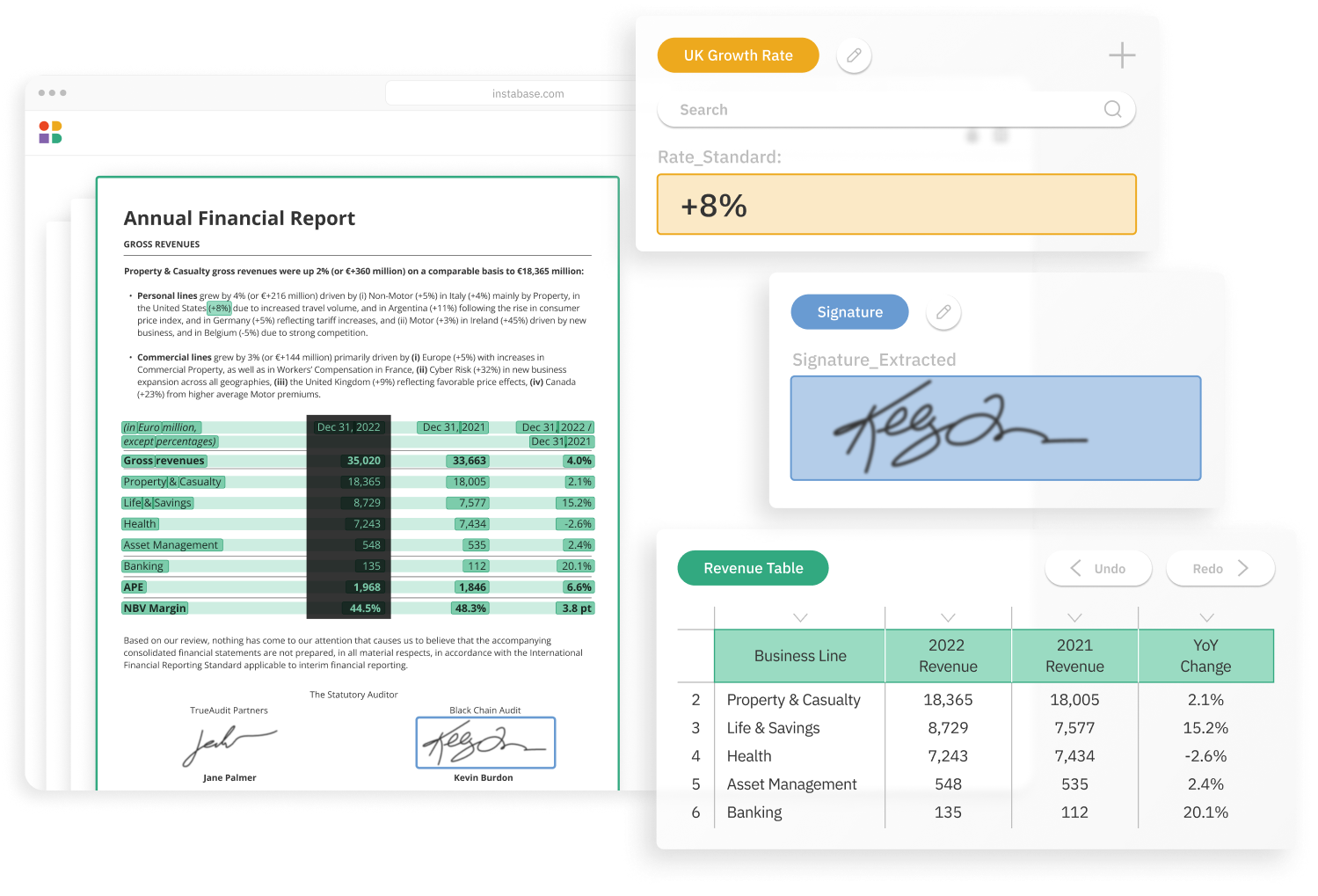
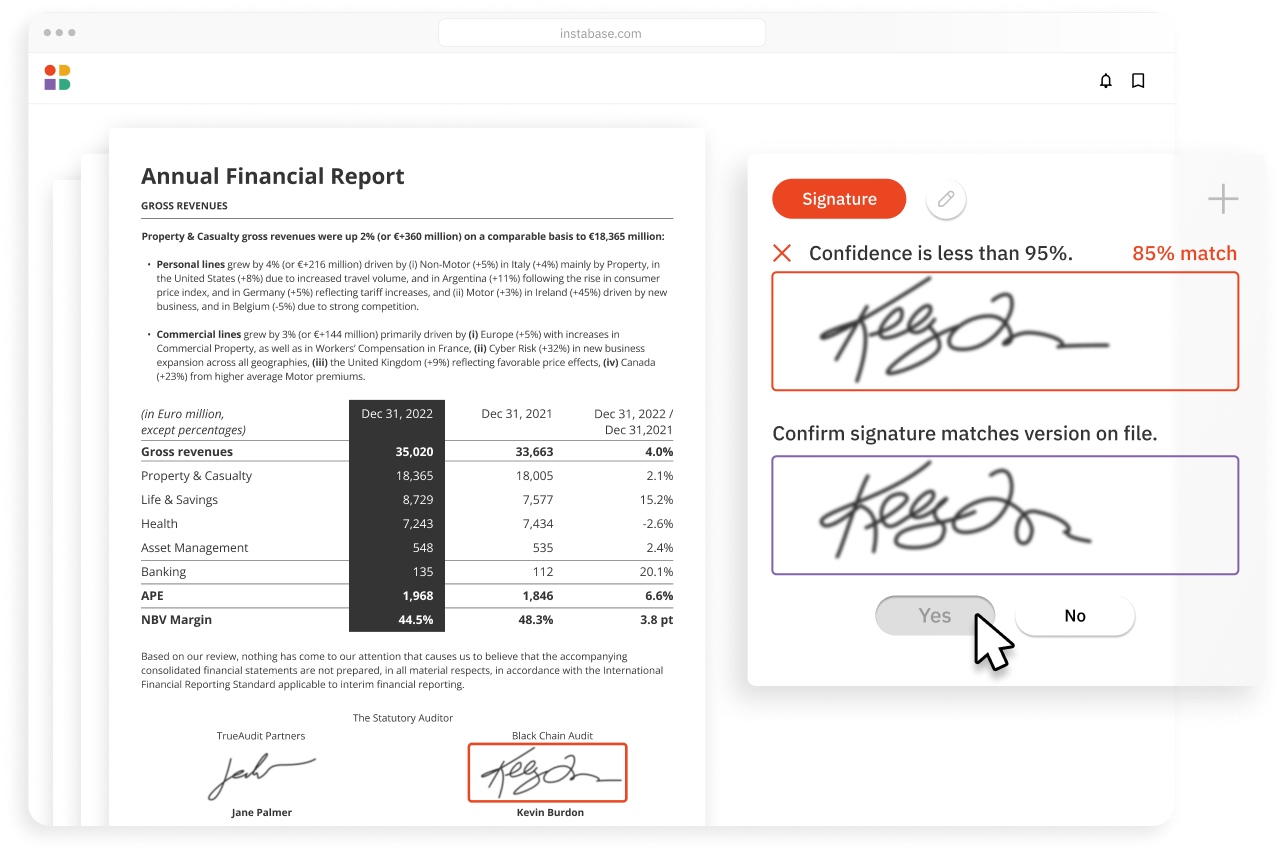
Use without any model training
- Out-of-the-box engine
- No model training required
- Configure fields & run
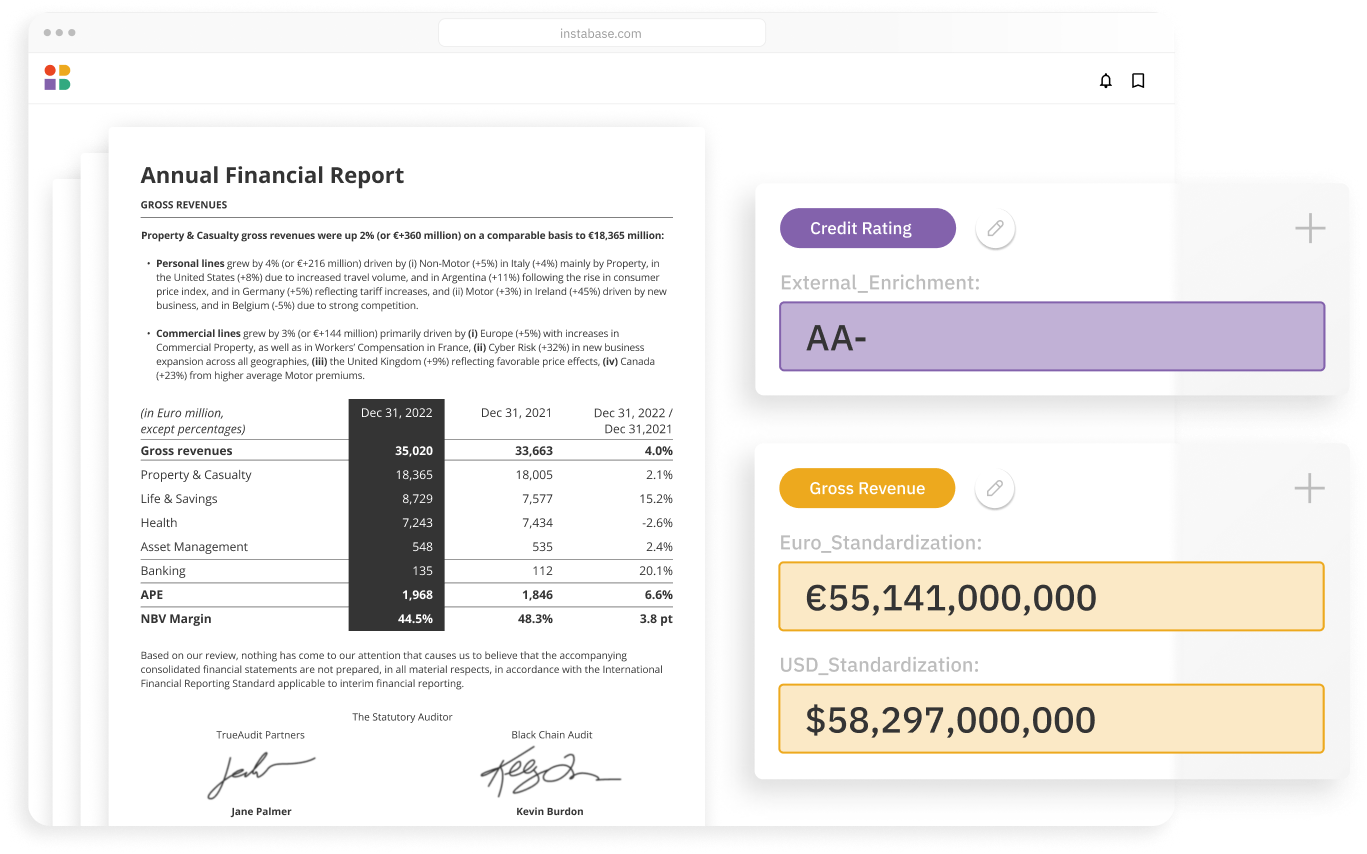
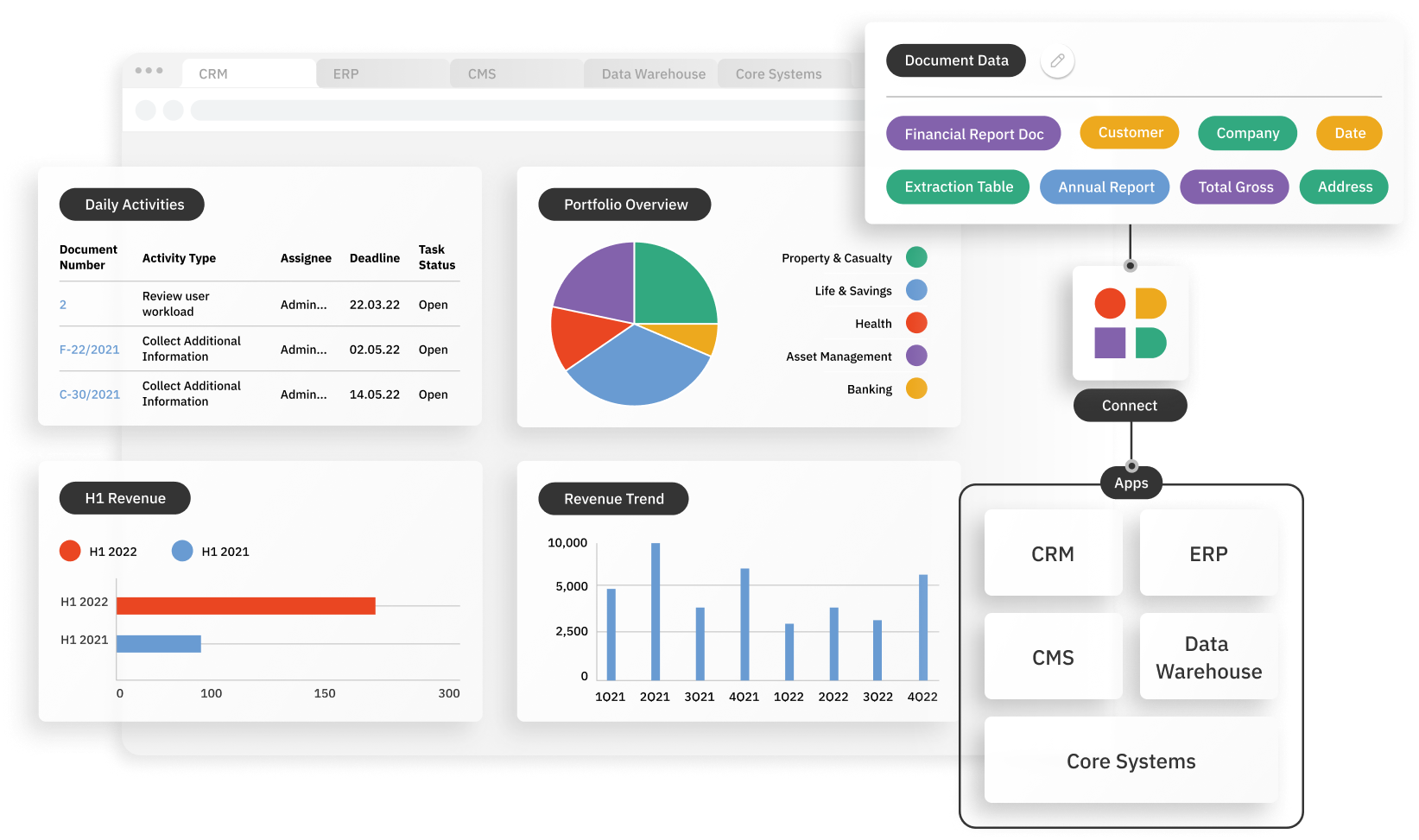
Easily embed into any workflow
- Scalable APIs
- Customize data schema
- Secure environment
How it works
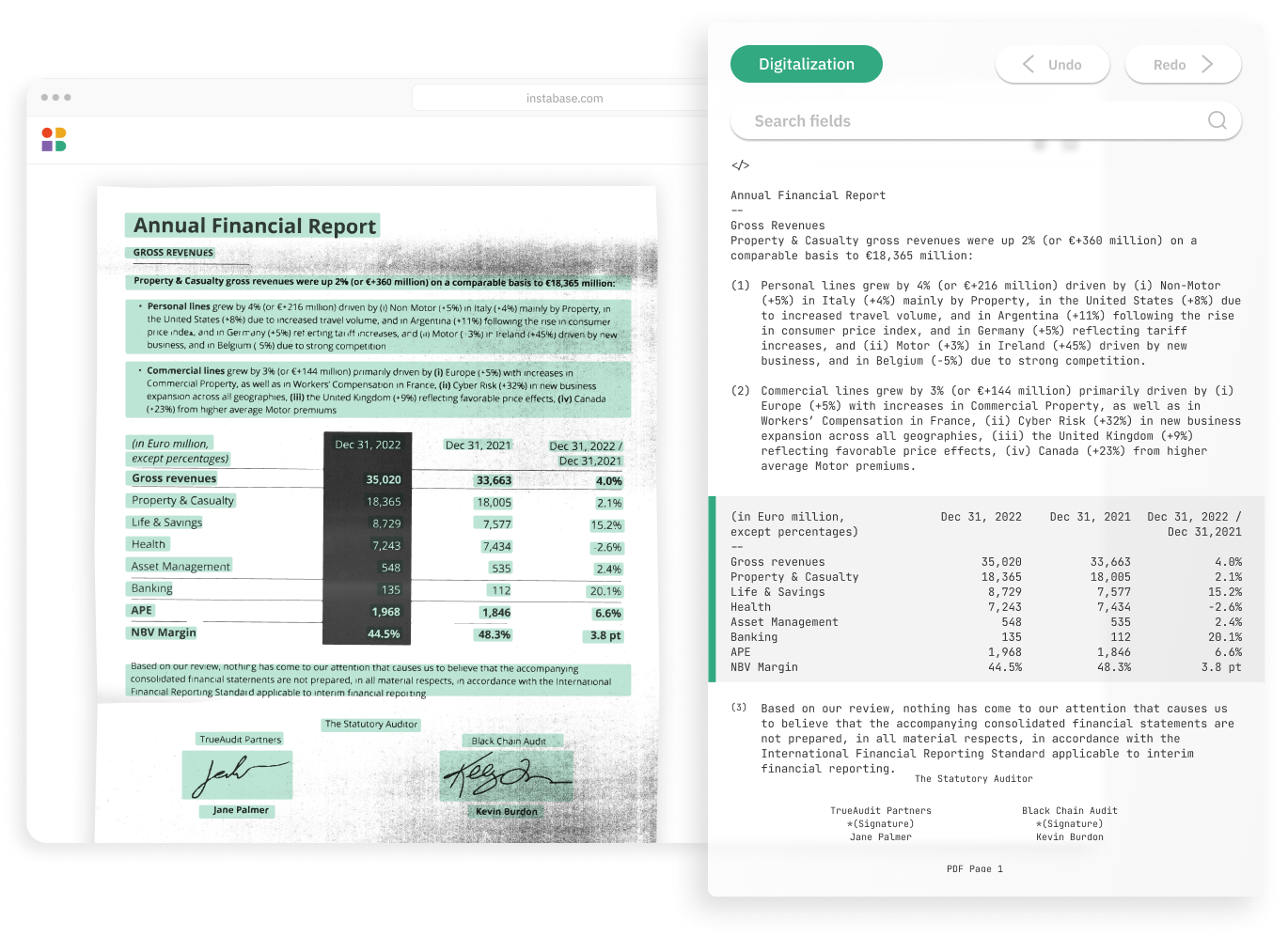
Instabase combines the most powerful technologies for every step of the process, so you can automatically understand any document for adjudication.