Utilization Management prevents fraud by assessing the cumulative usage of healthcare plans by patients. This analysis typically happens as part of claims adjudication, either to proactively or retrospectively prevent misuse or overpayment.
Instabase for Utilization Management
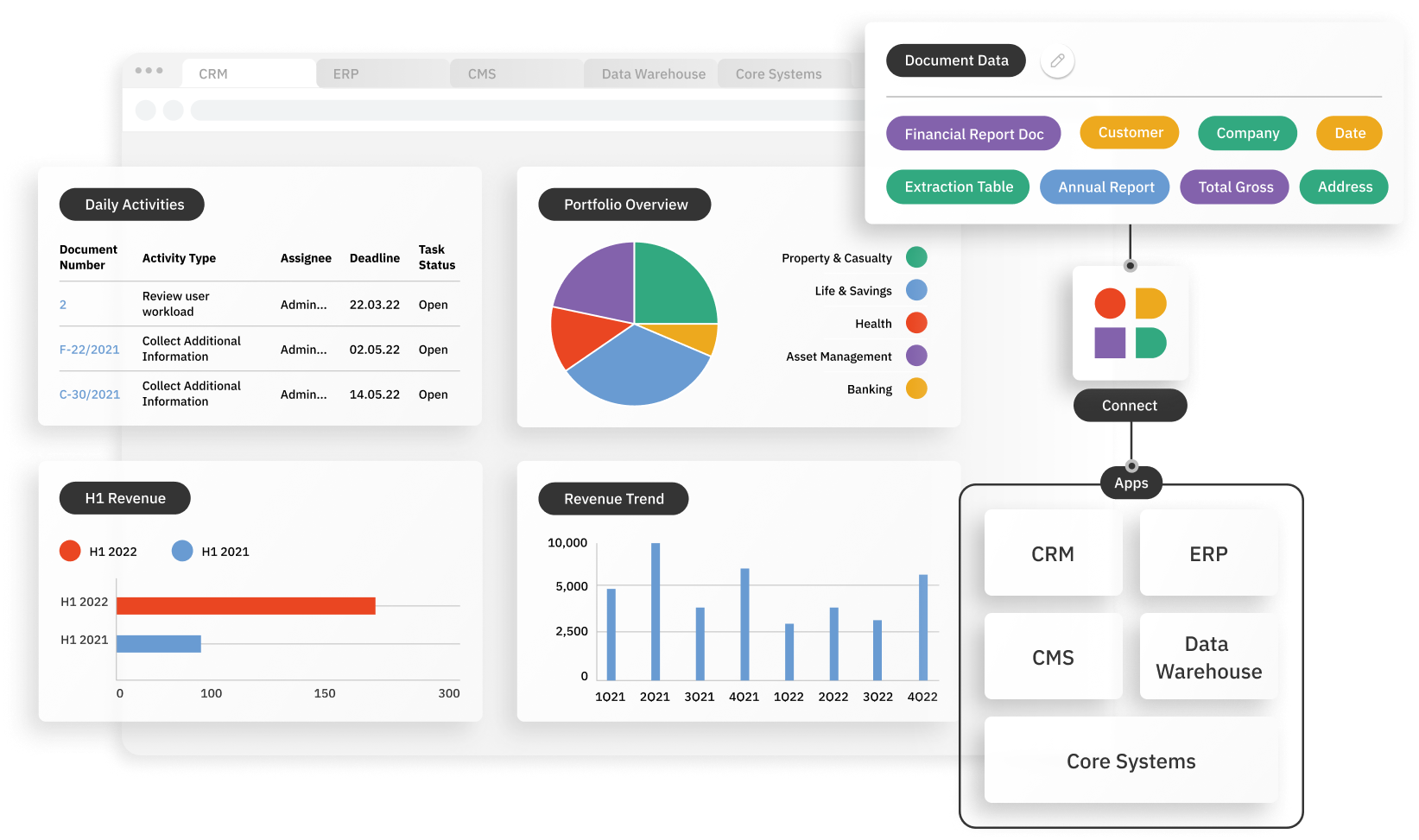
Instabase automates document understanding of all relevant documents for healthcare plan usage, streamlining utilization management in an end-to-end workflow.

Managing Healthcare Plan Utilization
Why Instabase?
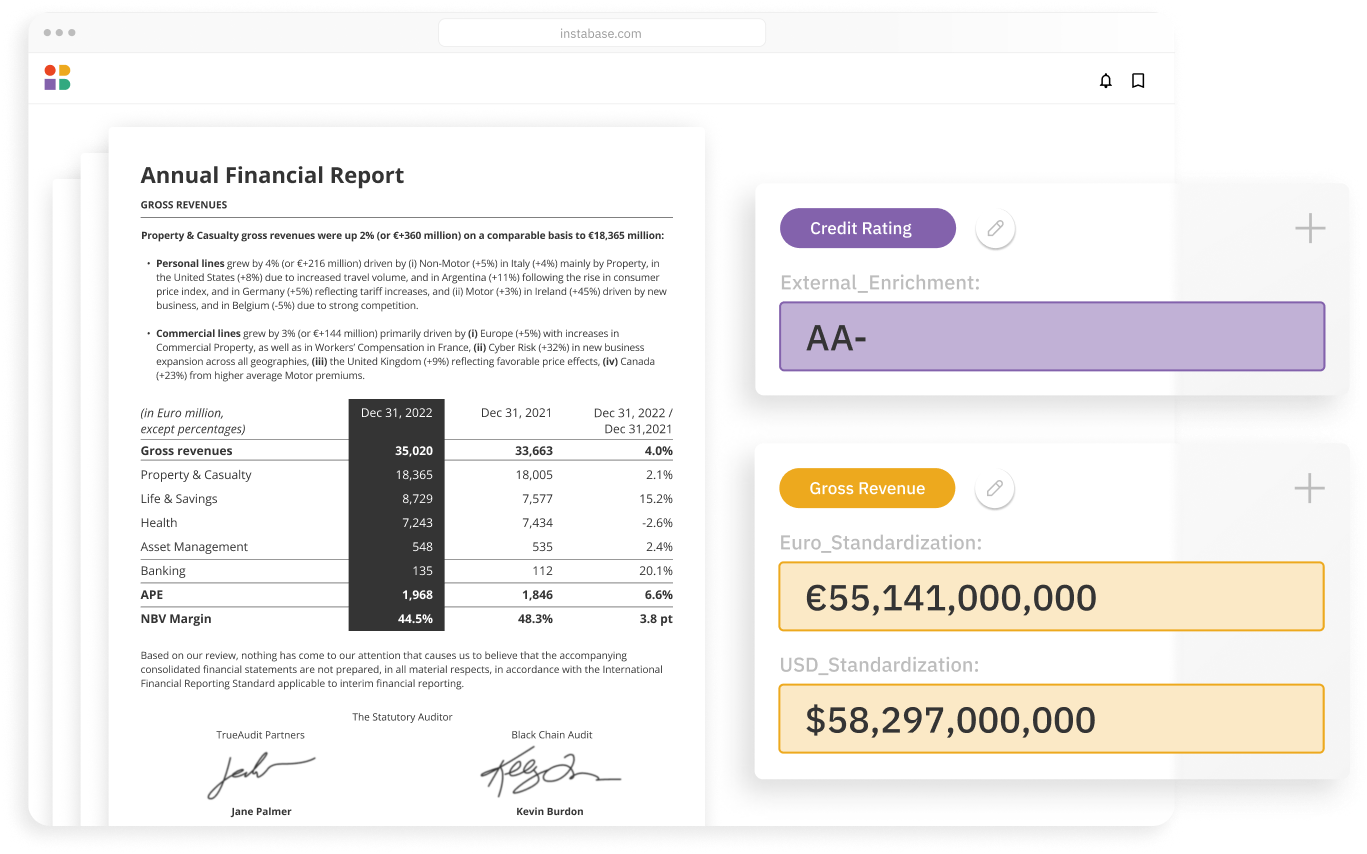
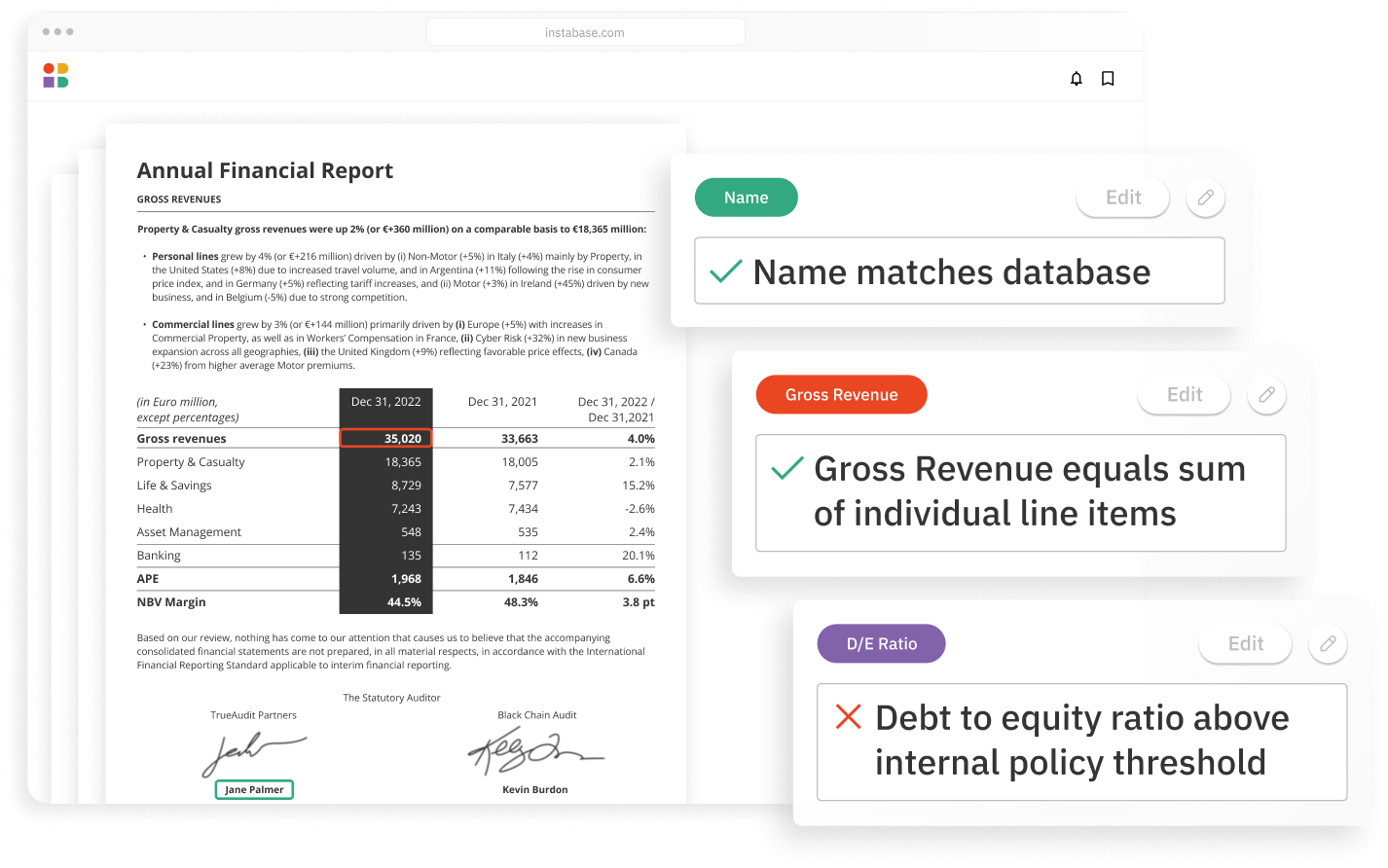
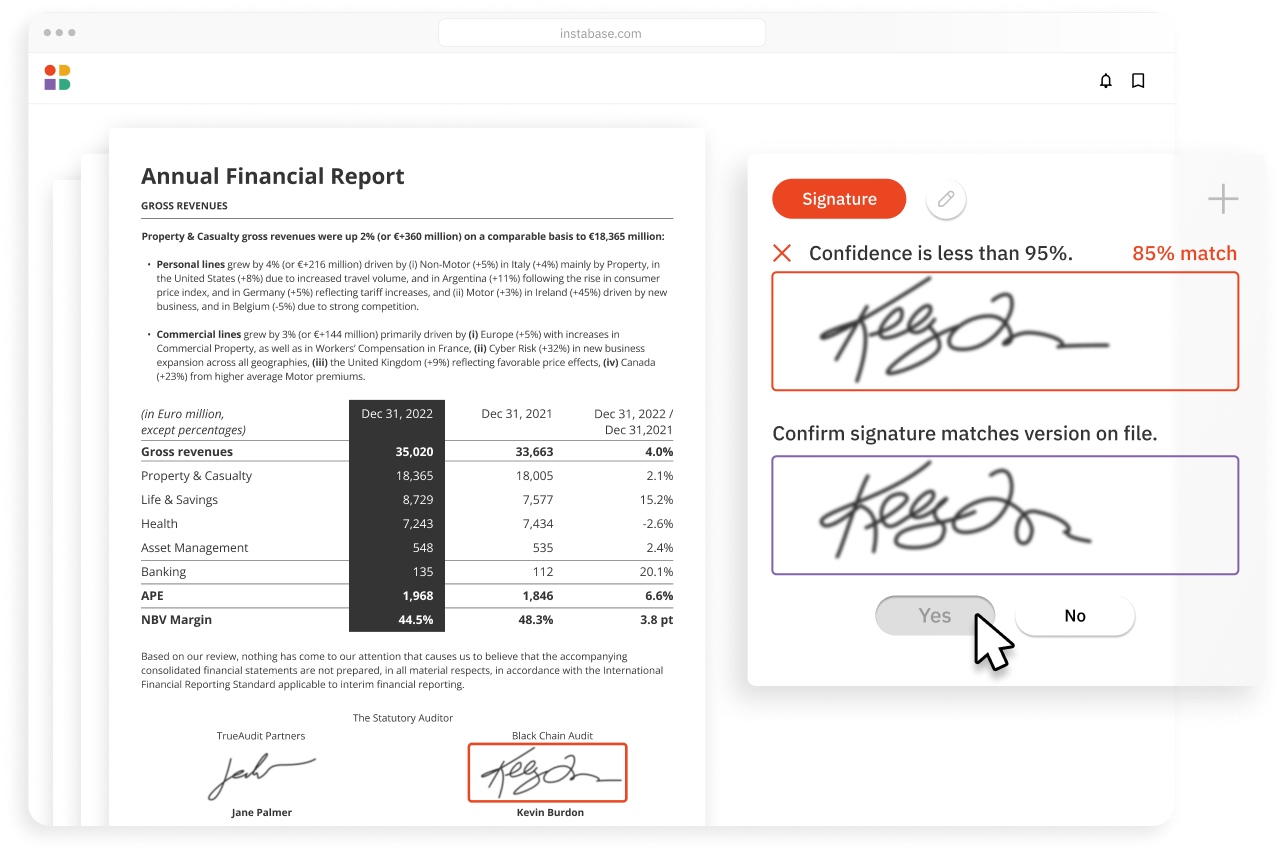
The Instabase Platform uses deep learning and natural language processing technology to help health insurance payors with utilization management by increasing accuracy and reducing processing times.
Accurately automate any document type
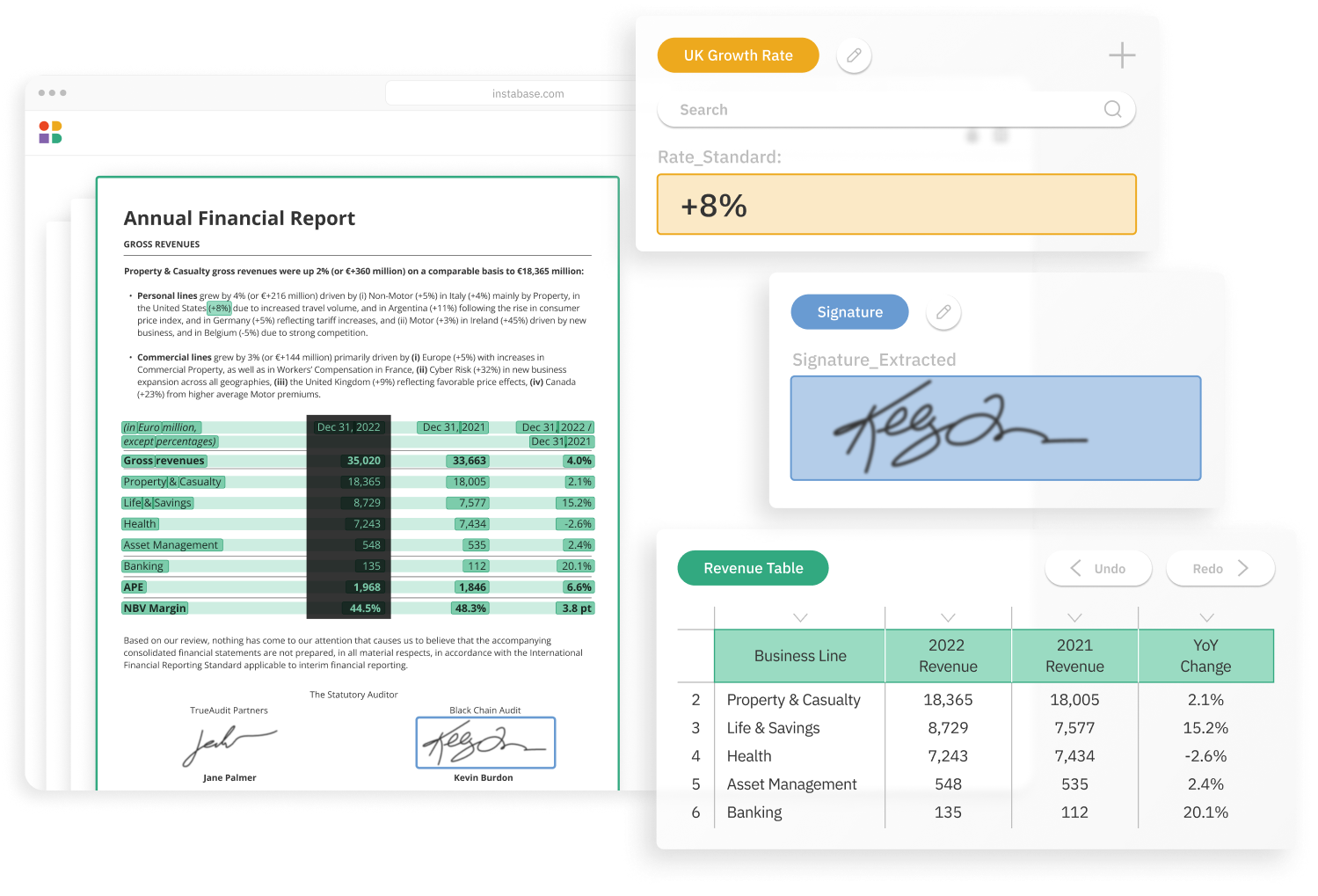
- Highly accurate extraction
- Any structure, any language
- Handwriting & printed
Use without any model training
- Out-of-the-box engine
- No model training required
- Configure fields & run
Easily embed into any workflow
- Scalable APIs
- Customize data schema
- Secure environment
How it works
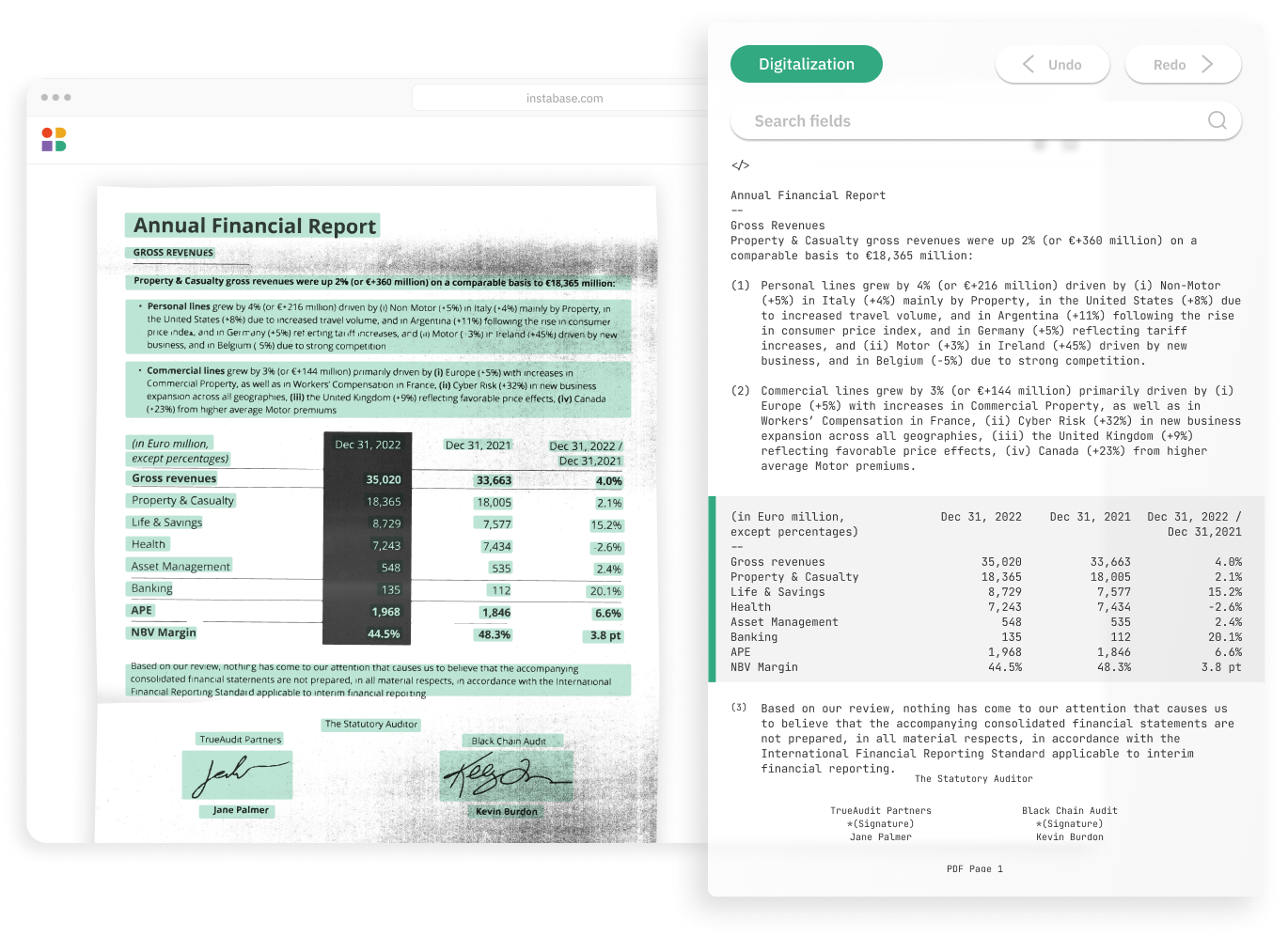
Instabase combines the most powerful technologies for every step of the process, so you can automatically understand any document.